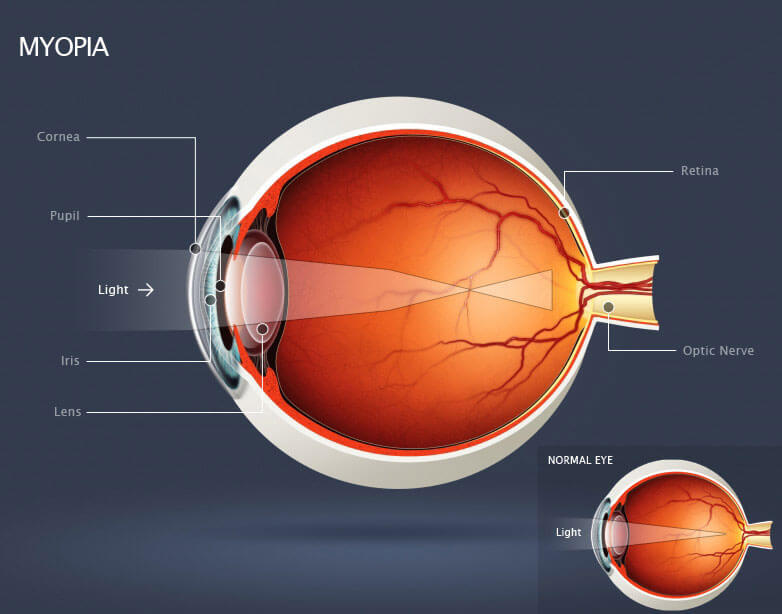
Myopia, also known as nearsightedness, is a common eye condition that affects millions of people worldwide. It occurs when the eyeball is too long or the cornea is too curved, causing light to focus in front of the retina instead of on it. As a result, objects in the distance appear blurry, while those up close are clear.
Myopia Symptoms
Symptoms of myopia can include squinting, headaches, eye strain, and difficulty seeing objects in the distance. Children with myopia may also have trouble seeing the board in school or playing sports that require good distance vision.
Diagnosing Myopia
Diagnosing myopia typically involves a comprehensive eye exam, which may include a visual acuity test, refraction test, and measurement of the shape of the cornea and the length of the eyeball. Early detection is important, as untreated myopia can lead to serious long-term complications.
Risk Factors Associated with Myopia
Risk factors for myopia include genetics, age, and certain environmental factors. Children with one or both parents who have myopia are more likely to develop the condition themselves. Spending a lot of time doing near work, such as reading or using a computer, may also increase the risk of myopia.
Long Term Implications of Myopia
Long-term implications of myopia can include an increased risk of cataracts, glaucoma, and retinal detachment. Additionally, high levels of myopia can lead to a condition called myopic maculopathy, which can cause permanent vision loss.
Myopia Prevention
Preventing myopia is difficult, as many risk factors are beyond our control. However, there is some evidence to suggest that spending more time outdoors and limiting near work may help reduce the risk of myopia in children.
Myopia Treatment Options
Treatment options for myopia include corrective lenses, such as glasses or contact lenses, and refractive surgery. Glasses or contacts work by bending light to focus it correctly on the retina, while refractive surgery reshapes the cornea to achieve the same result. Additionally, orthokeratology involves wearing special contact lenses that reshape the cornea overnight to temporarily improve vision during the day.
In conclusion, myopia is a common eye condition that can have serious long-term implications if left untreated. Early detection and treatment are important to prevent complications and preserve vision. While preventing myopia is difficult, certain lifestyle changes may help reduce the risk in children. If you are experiencing symptoms of myopia, it is important to schedule an eye exam with a qualified eye care professional.