The pachymeter is a diagnostic tool used in ophthalmology to measure the thickness of the cornea, the clear outer layer of the eye. This simple, yet powerful device has become an essential tool in the diagnosis and treatment of a variety of eye conditions.
The cornea plays a crucial role in vision by refracting light as it enters the eye. Any irregularities in its shape or thickness can lead to blurry or distorted vision. The pachymeter measures the thickness of the cornea, providing valuable information to ophthalmologists in diagnosing and managing corneal disorders.
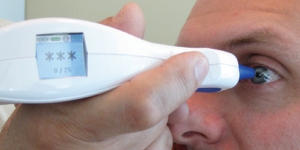
The pachymeter is a handheld device that uses ultrasound waves to measure the thickness of the cornea. The device emits a high-frequency sound wave that passes through the cornea and reflects back to the pachymeter. By analyzing the time it takes for the sound wave to return, the device can calculate the thickness of the cornea.
Uses for a Pachymeter
One of the most common conditions diagnosed using the pachymeter is glaucoma. Glaucoma is a condition where the pressure inside the eye increases, causing damage to the optic nerve and leading to vision loss. The pachymeter is used to measure the thickness of the cornea, which can affect the accuracy of intraocular pressure measurements. Thinner corneas can give falsely low pressure readings, while thicker corneas can give falsely high pressure readings. By taking the corneal thickness into account, ophthalmologists can more accurately diagnose and manage glaucoma.
The pachymeter is also used to monitor the progression of corneal disorders such as keratoconus. Keratoconus is a condition where the cornea becomes thinner and more conical in shape, leading to distorted vision. The pachymeter is used to measure the thickness of the cornea at various points, allowing ophthalmologists to monitor the progression of the disease and determine the appropriate treatment.
In addition to its diagnostic and monitoring capabilities, the pachymeter is also used to guide certain treatments. For example, during corneal transplant surgery, the pachymeter is used to measure the thickness of the donor cornea and ensure that it is a good match for the recipient’s cornea.
In conclusion, the pachymeter is a valuable tool in the field of ophthalmology. By providing accurate measurements of corneal thickness, it allows ophthalmologists to more accurately diagnose and manage a variety of eye conditions. With its ability to monitor the progression of diseases and guide treatments, the pachymeter has become an essential tool in the care of the eyes.