A keratometer is an ophthalmic instrument used to measure the curvature of the cornea, which is the clear front surface of the eye that covers the iris and the pupil. It is also known as an ophthalmometer, a corneal topographer, or a manual keratometer. The device is commonly used by optometrists and ophthalmologists to determine the refractive error and the astigmatism of the eye, as well as to fit contact lenses and assess the candidacy for refractive surgery.
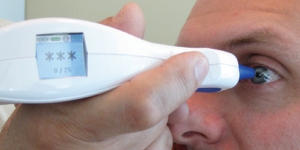
The keratometer consists of a pair of movable arms or spindles that are attached to a central axis, a light source, and a scale or dial. The patient sits in front of the instrument and focuses on a target while the examiner positions the instrument to align with the cornea. The light source projects a pattern of concentric circles or rings onto the cornea, which reflects back through the instrument and is viewed through a magnifying eyepiece.
The keratometer measures the radius of curvature of the cornea in two meridians, or directions, usually the horizontal and the vertical, but sometimes other oblique angles as well. The curvature is expressed in diopters, which is a unit of measurement of the refractive power of a lens. A diopter is defined as the reciprocal of the focal length of a lens in meters, so a keratometer measures the curvature of the cornea as if it were a lens.
Uses for a Keratometer
The keratometer is especially useful in diagnosing and correcting astigmatism, which is a common refractive error that occurs when the cornea is not perfectly spherical, but has a more oblong or elliptical shape. Astigmatism can cause blurred or distorted vision, especially at certain distances or angles. The keratometer can measure the degree and orientation of the astigmatism, which can be corrected with cylindrical lenses or toric contact lenses.
The keratometer can also be used to assess the corneal topography, which is the three-dimensional shape and curvature of the cornea. Corneal topography is important for detecting and monitoring corneal diseases, such as keratoconus, which is a progressive thinning and bulging of the cornea that can cause severe visual impairment. The keratometer can help in the early detection and treatment of keratoconus by mapping the corneal shape and thickness.
In summary, a keratometer is a valuable tool for measuring the curvature of the cornea and diagnosing refractive errors, astigmatism, and corneal diseases. It is a non-invasive and relatively simple instrument that can provide important information about the eye’s optical properties and guide the selection of appropriate treatments and corrective lenses. If you are experiencing vision problems or are considering contact lenses or refractive surgery, your optometrist or ophthalmologist may use a keratometer to assess your corneal curvature and help you achieve optimal vision.